Clinical Topic
Publication Date
February 16, 2021
Endocrinology Late Effects in Cancer Survivors: A Guide for Families
Advances over the years have allowed more children to “beat cancer” and survive into adulthood. Unfortunately, cancer treatments can cause health complications long after the cancer has been cured, called “late effects.” Not all cancer survivors are at risk for the same late effects. The specific consequences of cancer treatment depend on the chemotherapy used, as well as the type, location and extent of radiation or surgery needed to treat the cancer.
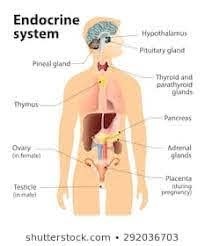
Some of these late effects could be related to problems with hormone production or action in the body. Hormones are chemical messengers that perform many important functions in the body. A pediatric endocrinologist is a doctor who specializes in the management of hormone disorders and is an expert in monitoring growth rate, pubertal development, thyroid function, and diabetes risk. Your child’s physician has referred your child to a pediatric endocrinologist so that they can take over screening for and management of possible endocrine consequences of pediatric cancers and treatments.
Why does this happen?
Some types of cancer require radiotherapy. Radiation targeted to the head and neck can affect areas in the middle of the brain called the hypothalamus and the pituitary gland. Together, the hypothalamus and pituitary gland are responsible for producing several hormones. These hormones are critical for growth, development, puberty, and metabolism. They also control several other endocrine glands, including the thyroid, adrenals, and ovaries/testicles. Radiation-damage to the hypothalamus- pituitary region or some of these endocrine glands can cause hormone-related problems. The effects of radiotherapy may occur many years later.
Most cancers require chemotherapy. Certain types of chemotherapy can affect hormone levels, particularly if they are ‘alkylating agents’ (like cyclophosphamide) or ‘heavy metals’ (like cisplatin). In particular, these can be directly harmful to the ovaries and testicles. Other agents such as ‘antimetabolites’ (like methotrexate) or ‘glucocorticoids’ (like prednisone or dexamethasone) may weaken the bones and cause increased risk of fractures. The higher the amount of such chemotherapies received over the years, the more likely it is for an individual to experience endocrine late effects related to these treatments.
Some types of cancer require surgery to remove the tumor. If an endocrine gland is close to the surgical area, a portion of the endocrine gland may be removed or damaged.
Some common childhood endocrine disorders are seen in long-term cancer survivors. These include an underactive thyroid gland, short stature, delayed or early puberty, failure of the ovaries or testicles (estrogen or testosterone insufficiency), weak bones, or underactive adrenal glands.
Hematopoietic stem cell transplants (HSCT), familiarly known as bone marrow transplants (BMT), are utilized to treat certain cancers and blood disorders. HSCT increases the risk of developing a future endocrine abnormality, especially because of the “conditioning” stage where chemotherapy and, in some cases, radiation are used to prepare for the transplant.
What are the symptoms of hormone issues?
Symptoms can vary based on the type of hormone problem, so it is important to be regularly seen by your physician for physical exams and laboratory testing. Below is a list of symptoms that may suggest specific endocrine concerns:
- Hypothyroidism/ underactive thyroid gland – dry skin, hair loss, decreased energy, feeling excessively cold, constipation, and irregular or heavy menstrual periods
- Hyperthyroidism/ overactive thyroid – sometimes this can be seen after very high doses of neck irradiation: feeling “hyper,” unintentional weight loss, fast heart rate, tremors, and difficulty sleeping.
- Second cancer affecting the thyroid, especially after neck irradiation: This can present with a lump / bump in the lower neck where the thyroid is located, or persistent lymph nodes felt in the neck. This usually occurs more than ten years after treatment.
- Adrenal insufficiency- fatigue, abdominal pain, nausea, weight loss, low blood sugar, low blood pressure, and dizziness
- Pubertal issues – early start of puberty (breast buds before 8 years of age in girls, pubic hair and increase in testicular size in boys before 9 years of age), delayed puberty (absence of puberty signs after 13 and 14 years of age in girls and boys respectively), abnormal menstrual periods, infertility
- Problems with bone strength, fractures, back pain
- Growth issues- short height, not growing at a normal rate
- Metabolic issues – high blood sugar, excessive thirst and urination (due to both diabetes “insipidus” and diabetes “mellitus”), overweight/ obesity, high cholesterol, high triglycerides
How common are these problems?
Endocrine abnormalities are common complications after childhood cancer. In a recent study of long-term childhood cancer survivors, more than half of the survivors had developed at least one endocrine-related problem. Developing an endocrine complication becomes more common as survivors get older.
Who will manage my long-term care?
It is important that your primary care physician is aware of your child’s cancer history (such as the chemotherapy agents and doses). This physician can coordinate the monitoring and care that is needed across multiple disciplines such as endocrinology, cardiology, and mental health. Your child’s primary care physician can monitor and screen for long-term complications related to the type of cancer therapy your child has received. If your child is suspected of having (or is diagnosed with) an endocrine disorder, your child will be referred to and followed regularly by a pediatric endocrinologist. Following the transition from pediatric to adult care, your child should continue regular monitoring visits with an oncologist, primary care provider, or endocrinologist depending on his/ her individual needs.
Is there a treatment?
If hormone deficiencies develop, they can be treated. These treatments may be needed life-long, as the effects of the cancer treatment are typically permanent. Whether there is an isolated hormone deficiency or multiple hormone problems, an endocrinologist can properly evaluate and manage each concern. Depending on the hormones affected, treatment may include pills, shots, and patches.
For more information: please visit survivorshipguidelines.org.
